April Turner, Graduate Student and Public Policy Intern, North Carolina Center for Nonprofits
What Is It?
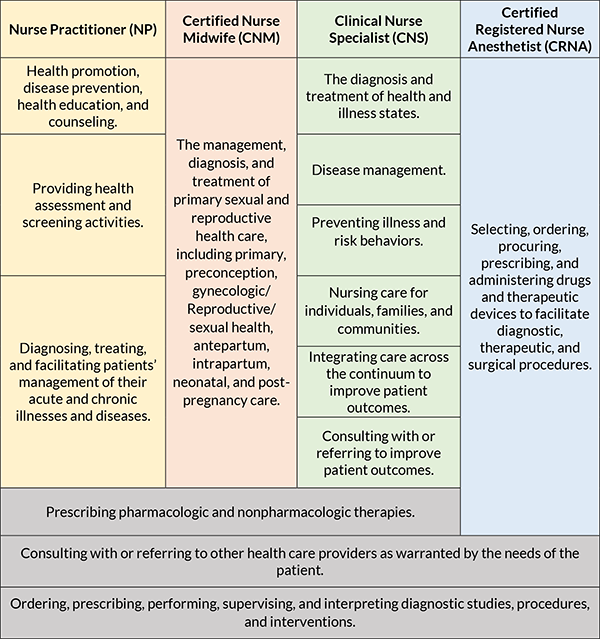
The SAVE Act (SB 249) was introduced on March 11, 2021 and is intended to “deliver safe, accessible, value-directed, and excellent (save) health care throughout North Carolina by modernizing nursing regulations.” It enables Advanced Practice Registered Nurses (APRN) to practice without Physician supervision, within one of four roles: Nurse Practitioner, Certified Nurse Midwife, Clinical Nurse Specialist, and Certified Registered Nurse Anesthetist.
APRN Roles and Responsibilities
As outlined in SB 249, the four roles and responsibilities are as follows. These responsibilities are in addition to the roles and responsibilities for Advanced Practice Registered Nurses.
History and Current Status
Full practice authority (FPA), or the ability for an advanced practice registered nurse (APRN) to practice to the full extent of their license, was first authorized in 1994. The National Council of State Boards of Nursing notes that currently 24 states (including D.C. and Guam) have reduced limitations on the scope of practice (SOP) of APRNs. The National Council of State Legislatures outlines the varying restrictions on SOP across the US within three main policy areas. Restrictions vary from having a physician supervisor outline what procedures an NP may perform independently and what procedures they must get a consultation for, to completing a “transition to practice” period before getting to practice independently, to practicing without supervision. Additionally, restrictions of the same nature limit the prescribing ability of APRNs as well as whether they are also recognized as primary care providers. No state to pass FPA or loosen restrictions has repealed their decision.
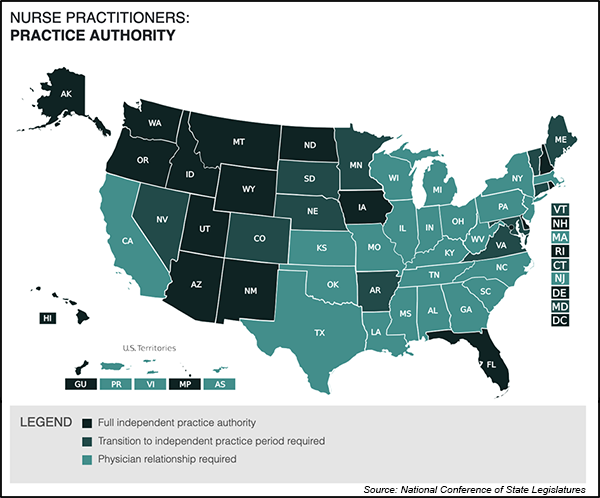
North Carolina has dual regulation regarding the SOP of APRNs; The NCSBN notes that full practice authority is granted to those APRNs working within the Veterans Affairs System, Indian Health Services, and the Military. “CRNAs are stationed around the world as the primary providers of anesthesia in the military, administering safe, high-quality anesthesia care to our nation’s soldiers,” included the American Association of Nurse Anesthesiology. All other APRNs are restricted to the regulations regarding scope of practice.
Physician Supervision
NC Health News provides information regarding current supervision laws. Currently, APRNs can practice but are required to have a supervising physician. Per NC law, the physician is not required to be in the same vicinity; Physicians and NPs may be geographically separated. APRNS pay a preceptor or supervisor to conduct a chart review and consult on cases as needed.
Health Professional Shortages
North Carolina continues to face workforce shortages, namely in the health professions. Of NC’s 100 counties, 87 have a primary care, dental, and mental/behavioral health care shortage, according to the National Conference of State Legislatures. These shortages have only been exacerbated by the COVID-19 pandemic. Areas designated as Health Professional Shortage Areas (HPSA) are those that have a shortage of primary, dental, or mental health care providers. HPSAs are designated based on population-to-provider ratio, percent of population below 100% of the Federal Poverty Level (FPL), and travel time to the nearest source of care outside the HPSA designation area.

COVID-19 Pandemic
During the coronavirus COVID-19 pandemic, many states moved to temporarily expand the scope of practice for APRNs to address the worsening shortage of health professionals. According to NCSBN, a total of 12 states removed their Collaborative Practice Agreements (CPA). Others issued licensure waivers and telehealth waivers. On the federal level under the Trump Administration, the Centers for Medicare and Medicaid Services (CMS) approved its 24th state Medicaid waiver request, the Department of Health and Human Services issued a letter urging the temporary removal of scope of practice barriers, and the Veterans Health Administration granted CRNAs full practice authority. (Prior to the pandemic, the VHA had already expanded SOP for NPs, CNMs, and CNSs).
Pros and Cons of the SAVE Act
There is a wide body of research both in favor of and against full practice authority for each of the four roles. The primary areas of concern are quality of care, access to care (re: the current health professional shortage), education, cost.
| Pros | Cons | |
|---|---|---|
|
Quality of Care |
Increased access to midwifery care (including through CNMs) is correlated with a reduction in interventions, lower neonatal deaths, increased breastfeeding, and increased vaginal delivery (American College of Nurse-Midwives). CNM care is associated with reduced adverse outcomes and shorter newborn hospital states, without compromising maternal or child health (AARP). |
Granting CRNA full practice could create a two-tier system of care, one tier inclusive of physician supervision and one without (NC Society of Anesthesiologists). The presence of a physician anesthesiologist prevented 6.9 deaths per 1,000 patients in which an anesthesia-related or surgical complication occurred (NC Society of Anesthesiologists). |
|
Access to Care |
According to a consensus study report, if FPA was enacted nationally, the number of Americans living in a county designated HPSA would decrease by 70% overall and by 65% in rural areas (Duke University School of Nursing). Nurse Practitioners are more likely to practice in rural areas (John Locke Foundation). FPA has been found to increase participation in Medicaid (NC Society of Anesthesiologists). |
Anesthesia is provided as part of a scheduled surgical procedure. As such, a physician is always directly involved, therefore eliminating the requirement for physician supervision would have no effect on access to healthcare as they must be present regardless (NC Society of Anesthesiologists). |
|
Education |
Nurse Anesthetists undergo 5-7 years of education (following high school) as compared to the nearly 14 years of total education for Physician Anesthesiologists (NC Society of Anesthesiologists). NPs are not required to complete a residency, whereas Physicians are required to complete 3-7 years of residency (Karen Smith, MD, FAAFP). NPs complete a total of 500-720 hours of clinical training in contrast to the 10,000-16,000 hours required for Physicians (Karen Smith, MD, FAAFP). NP education is not standardized; Physician education is standardized and proven (Karen Smith, MD, FAAFP). |
|
|
Cost |
FPA has the potential to achieve health care system savings of at least $433 million, and would create at least 3,800 new jobs, generating more than $20 million in tax revenues (AARP). The cost of training NP is estimated to be 20-25% less than for physicians (John Locke Foundation). The cost of training CRNAs is approximately seven times less than for anesthesiologists (John Locke Foundation). APRNs provide the same services as MDs but at a lower rate of compensation (John Locke Foundation). |
With current supervision requirements, both NPs and PAs are compensated for their involvement in the provision of care; two clinicians are compensated when only one is needed (AARP). Anesthesiologist-led care significantly reduced costs compared to the nurse model (NC Society of Anesthesiologists). |
How might this benefit or challenge NC nonprofits?
The SAVE Act has the potential to combat the workforce shortage, especially in rural communities. Studies have shown that states with FPA have a higher supply of APRNs. Nevada experienced a 33.4% growth in practicing APRNs in the years after granting FPA. Should more APRNs practice in NC, there will be greater access to care, limiting the strain on nonprofits’ resources to address the health and wellness needs of residents. Having sufficient practitioners could also combat the closure of rural hospitals by decreasing uncompensated care through greater appointment availability. Further, direct financial support would increase. According to Rose Hoban with NC Health News, if Medicaid is expanded in any capacity, granting APRNs full practice authority would increase the supply of health professionals to meet the demand that would result from expansion.
There is conflicting research on the education of CRNA APRNs as compared to Physician Anesthesiologists, and its impact on quality of care. There is also conflicting research regarding the quality of care provided by APRNs (all four roles). Many studies claim there is a difference, yet others that there is no difference. If there truly is a difference in quality of care (based on education and training in the case of CRNAs) nonprofits may need to utilize more resources to combat outcomes in the chance they are negative.
The economic benefits associated with the SAVE Act would greatly benefit nonprofits. According to AARP, passage of the SAVE Act can provide at least $433 million in savings to the health care system. It also has the potential to create at least 3,800 new jobs, which would generate tax revenues greater than $20 million.
HB 149
On May 24, House Bill 149: Expanding Access to Healthcare was introduced. It addresses a few components of the SAVE Act. Definitions are added to provide further clarity regarding APRNs, their responsibilities, and the four roles; clarification is provided regarding the practice of APRN versus the practice of medicine, surgery, and dentistry; and joint supervision of APRNs by the NC Medical Board and NC Board of Nursing is repealed, to name a few.
Currently, the authority to regulate the prescribing power of APRNs is held jointly by the NC Medical Board and the NC Board of Nursing (BON). Per HB 149, sole authority of regulation will be granted to the Board of Nursing. The BON will be responsible for supervising the prescription of drugs by APRNs. HB 149 also clarifies that practicing as an APRN is distinct from the practice of medicine, surgery, and dentistry. The bill does not make any modifications on APRN scope of practice, nor does it eliminate the requirement of supervision by a Physician.
